Population health is a popular phrase in the NHS, but what does it really mean and how can we, as commissioners, providers and health systems, benefit from it? Dr Nick Pulman explains.
At its most basic, Population Health Management (PHM) uses data about patients – be that health, social care, education, demographic or housing data – to understand the needs of a population. Its main purpose is to help commissioners and clinicians identify groups of patients, at a local, regional and national level, and match them to the correct intervention to improve health outcomes.
PHM includes two key tools – segmentation and stratification.
- Segmentation essentially means dividing patients into groups. This could be by common illness, group of illness, age or other factors.
- Stratification is simply another term for sorting, but there is more analysis applied here as the sorting is into risk factors. This is where PHM offers real potential. As well as identifying those most at risk of unplanned admissions, stratification is giving us a better understanding about risks associated with certain conditions. For example, we now know that patients with a long-term condition are likely to have approximately seven comorbidities. Knowing that allows us to anticipate need and plan more holistic preventative care. Similarly, while traditionally there has been a sense that older patients are more costly, risk stratification has shown that number of conditions has a much greater impact on a patient’s use of NHS resources.
Supporting health systems
As clinicians, we are used to specific and controlled analysis. When it comes to managing a population, however, the task is much more complex. Traditional tools used to identify needs such as average age and socio economic group are blunt, as are like-for-like comparisons of practice performance and spend. PHM provides a much richer and more accurate understanding of your patients which is essential when it comes to allocating resources effectively.
For example, in Leicestershire, Primary Care Networks have been commissioned to provide clinical support behind a model of more intensive community nursing. Funding would normally be allocated on a population or age basis. Instead, PHM has been used to allocate funds based on risk linked to multi morbidities.
PHM is also being used to develop a business case for new services. For example, Arden & GEM has developed a localised population analysis tool for Norfolk for use by the STP, PCNs and individual practices. We’ve worked with the PCNs to understand the impact of low-level long-term conditions on mental health risk, which has helped build a case for the introduction of interventions such as social prescribing support and digital self-care tools.
When the local STP wanted to look at the best locations for maternity hubs, the segmentation model was used to accurately profile likely births, likely needs of mothers and their distance from potential maternity hubs. The output was a clear recommendation of where to site maternity hubs to ensure the highest level of access among those who would need them most.
PHM is not the complete solution
Despite these positive examples, it’s fair to say that while PHM is wonderful tool waiting to be used, its potential is not yet fully understood. But it is also not a solution in its own right. Unless you have an intervention planned, analysis is likely to be of little use.
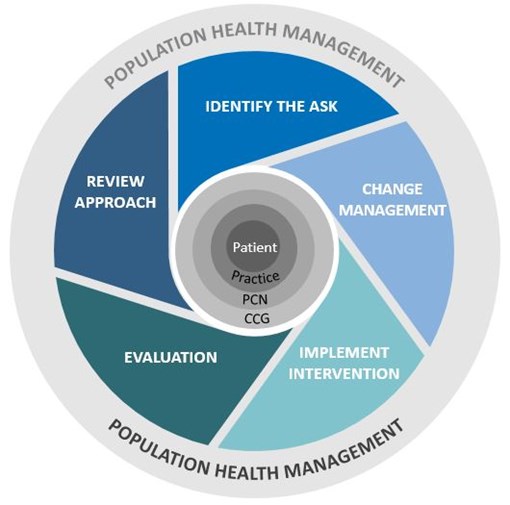
PHM works best as a cyclical process. It starts with identifying what you want to know – which patients are you looking to target and/or what problem are you trying to solve. And what changes or new interventions do you plan to introduce? Careful thought also needs to be given at the outset to how you will evaluate the impact of any change so that you can review your approach accordingly.
Interest in PHM is growing rapidly and it will be exciting to see how it can support us in moving towards more preventative care.
This blog was originally written for Healthcare Leader. To full the view version, visit their website.

