Did you know that humans make, on average, 35,000 decisions a day? For senior executives, that number is even higher.
Making the right decisions in publicly funded health systems is crucial for everyone, as it drives improved quality of care, reduces inequalities in access, and enables productive and efficient services. This remains a fundamental challenge for every employee and senior leader across health and care systems today.
In the current climate, ensuring resources are invested wisely within the NHS is paramount. While it is evident that better decisions lead to better outcomes and performance, the challenge lies in enabling the entire organisation and its partners to make better decisions together. Additionally, it is essential to measure the quantifiable benefits of these improved decisions for patients, staff and taxpayers.
This article, based on research across various industries, explores three key questions:
- What are the characteristics of good decisions?
- How can decisions be connected for value?
- What are the enablers of systemised value-based decision-making?
The health and care context
In health and care, decisions significantly impact our ability to treat people in need, influencing the length and quality of life and overall wellbeing. Research in social sciences, economics and psychology highlights the importance of improving decision-making across four main areas.
Quality of decisions
- Decisions are framed against clear objectives, with benefit criteria and measures for impact
- Relevant and reliable information is provided across multiple measures to enable the decision.
Impact of decisions
- Outcomes from each decision choice are clear, as are trade-offs between factors such as money, capacity, workforce, performance, outcomes, quality
- Decisions are made at the right level for the impact required, at an operational or strategic level.
Action orientated
- Decisions can be acted on within a timeframe that enables the benefits to be delivered.
Productive
- Decisions are made efficiently – the organisation sets out how and where decisions are made
- Increasing the percentage of available management time for making decisions.
Improving decision-making processes alone won't enhance the value delivered by these decisions. Confidence in resource management and optimal results requires connecting decisions across the operational chain to achieve value.
Connecting decisions for value
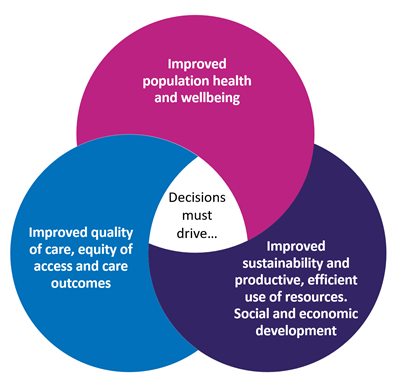
The NHS has a legal duty, known as the Triple Aim, to consider the impact of decisions on:
- Increasing the health and wellbeing of the population it serves, including addressing inequalities in health and wellbeing
- Ensuring the quality of healthcare services for all the population it serves, including addressing inequalities in benefits from those services
- Sustainable and efficient use of NHS resources.
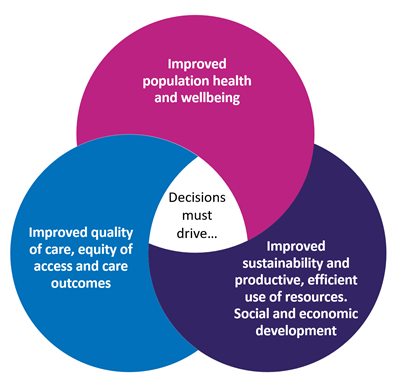
But how can decisions be better connected to deliver these aims?
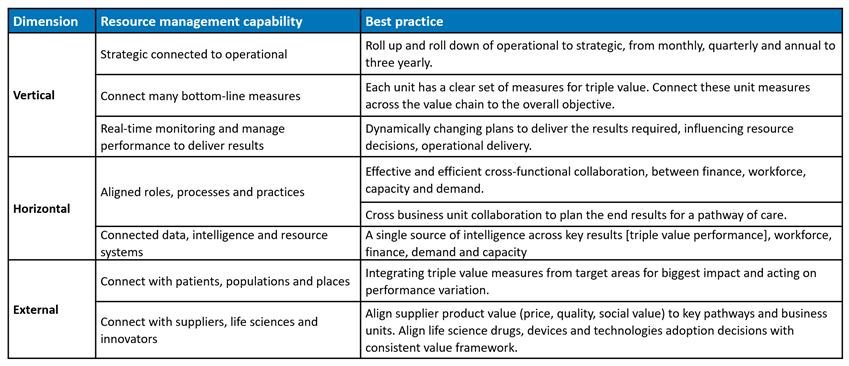
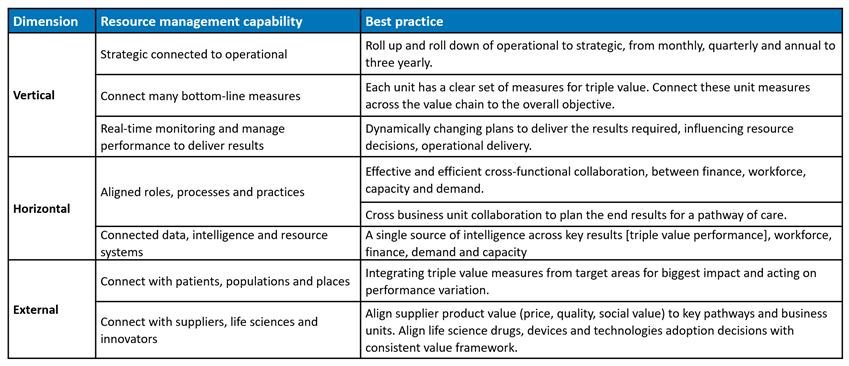
A highly connected organisation focuses on ensuring resources are managed optimally through interconnectivity of data, intelligence, processes, governance, and systems aligned across three dimensions:
Vertically – from board to operations, strategic to operational
Horizontally – across functions or delivery units working together to deliver end results, such as a pathway of care
Externally – serving populations and places to deliver value for specific population groups, e.g. frail elderly or young black males with mental illness in a neighbourhood.
What does being connected across these dimensions look like?
Enabling decisions through enterprise resource management
Industry has long recognised the importance of integrated planning, advanced intelligence and decision functions within their organisations. Indeed, research papers abound with empirical evidence which demonstrates the significant impact of integrating real-time operational information systems and business planning on key results such as market share, sales, efficiency and satisfaction.
Key improvements observed include:
- Increasing revenue by 52%
- Improving forecast accuracy by 31%
- Enhancing perfect order and customer service by 31%
- Better supply planning and schedule adherence by 31%
- Improving new product launch by 28%
- Reducing inventory by 27%
- Better translation of demand into procurement requirements by 21%
- Improved capital planning and asset management by 21%
- Developing and executing demand-shaping programs by 20%
- Enhancing logistics planning by 19%
- Improving asset utilisation by 17% (Palmatier & Crum, 2013)
NHS organisations seeking assurance on connected resource management, require an enterprise-wide connected planning function, with integrated data and intelligence, across processes and accountabilities. Supported by a dynamic system capability which can map key resource drivers, decision points and results.
In NHS Arden & GEM, our aim is to integrate intelligence from demand, activity, capacity, finance and workforce to the performance results delivered and required. Aligning these with decision metrics that reveal opportunities for improved operational and strategic decision-making, for investment, performance and productivity, and patient access.
Our proof of value work at present includes a whole organisation or system-wide integrated business planning platform, with a focus on priorities such as elective or urgent care results, workforce planning and productivity planning.
Early results from connected decisions in the NHS
These examples illustrate the tangible benefits of connected decision-making in the NHS, highlighting the potential for improved productivity, efficiency, and collaboration across health and care systems.
Example 1: Financial planning and productivity gains
By integrating financial planning metrics, NHS Trusts have demonstrated significant productivity gains. For instance, one Trust's approach to financial planning has resulted in each full-time equivalent (FTE) employee saving 3-4 days per month previously spent on manually aggregating and adjusting data for resubmission into their general ledger. This translates to a 20% productivity gain each month, regardless of the organisation's size. Furthermore, by connecting finance with workforce data, budget holders are saving 20% of their time previously spent on spreadsheets, allowing them more time to advise operational staff effectively.
Example 2: System demand and capacity planning
An Integrated Care System (ICS) has implemented an integrated business planning platform. This platform replicates NHS England planning submissions with connected assumptions and scenarios, consolidating ICS-wide reporting. The pilot project demonstrated several benefits:
- A system-wide view of demand and capacity on beds and services for acute, community, local authority, and hospice services
- Dynamic reports viewed across different dimensions and levels of detail to improve operational efficiency
- Forecasting capabilities allowing users to adjust factors like admissions and capacity to understand their impact on demand and capacity shortfall
- Improved collaboration between system partners, creating a shared understanding and facilitating targeted actions to improve patient/service user flow through the system.
In conclusion, effective decision-making is vital in publicly funded health systems to ensure improved quality of care, equitable access and efficient use of resources. By focusing on connected decision-making, organisations can enhance the overall value delivered to patients, staff and taxpayers. The three critical elements discussed—characteristics of good decisions, connecting decisions for value, and enabling decisions through enterprise resource management—provide a comprehensive framework for achieving these goals.
To truly transform decision-making processes, NHS organisations need to integrate data intelligence with key processes, establish clear accountability and adopt dynamic system capabilities. This integrated approach can significantly improve operational and strategic decision-making, driving better outcomes across the board.
We are committed to building systems that integrate data from various sources, connecting these to the performance results required. Our integrated business planning platform aims to improve investment, performance, productivity and patient access.